The fluid and electrolyte hesi case study presents a compelling opportunity to delve into the complexities of fluid and electrolyte imbalances. This case study offers a unique lens through which we can explore the assessment, diagnosis, and management of these critical conditions.
As we navigate this case study, we will encounter a patient with a complex medical history and a constellation of symptoms that point to potential fluid and electrolyte imbalances. Through a comprehensive analysis of the patient’s presentation, laboratory findings, and treatment plan, we will gain a deeper understanding of the underlying pathophysiology and the principles guiding their management.
Fluid and Electrolyte Imbalances: Fluid And Electrolyte Hesi Case Study
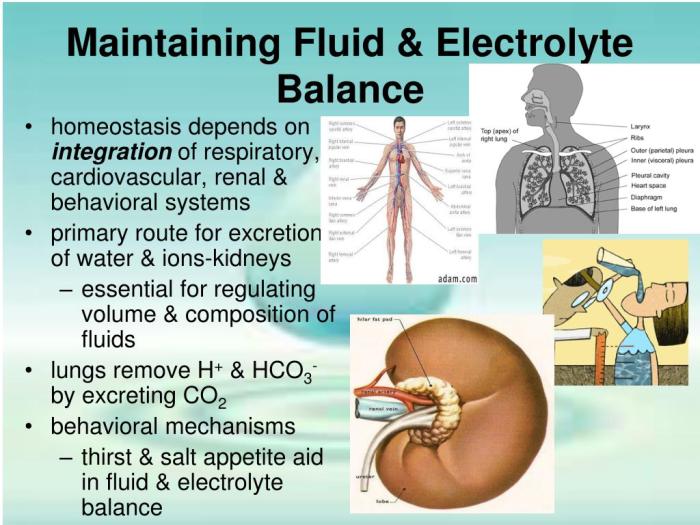
Fluid and electrolyte imbalances are common clinical problems that can have serious consequences if not promptly recognized and treated. This case study will provide an overview of fluid and electrolyte imbalances, their causes, and management.
Patient Presentation
A 65-year-old male with a history of hypertension and diabetes presents to the emergency department with complaints of weakness, nausea, and vomiting. He has been experiencing these symptoms for the past 24 hours. His vital signs are as follows: blood pressure 90/60 mmHg, heart rate 110 bpm, respiratory rate 20 breaths per minute, and temperature 38.5°C.
Physical exam reveals dry mucous membranes, poor skin turgor, and decreased capillary refill time. Laboratory results show the following:
- Sodium: 130 mmol/L
- Potassium: 3.5 mmol/L
- Chloride: 95 mmol/L
- Bicarbonate: 20 mmol/L
- BUN: 30 mg/dL
- Creatinine: 1.2 mg/dL
Fluid and Electrolyte Assessment
The patient’s fluid balance is negative, as evidenced by his dry mucous membranes, poor skin turgor, and decreased capillary refill time. His electrolyte levels are also abnormal, with hyponatremia (sodium<135 mmol/L), hypokalemia (potassium <3.5 mmol/L), and hypochloremia (chloride <98 mmol/L). His bicarbonate level is also low, indicating metabolic acidosis.
Etiology and Differential Diagnosis, Fluid and electrolyte hesi case study
The most likely cause of the patient’s fluid and electrolyte imbalances is gastrointestinal losses due to vomiting. Other possible causes include renal losses, endocrine disorders, and medications.
Treatment Plan
The initial treatment plan for the patient includes:
- Intravenous fluid resuscitation with normal saline
- Potassium replacement
- Sodium bicarbonate replacement
Monitoring and Evaluation
The patient’s fluid balance and electrolyte levels should be monitored closely during treatment. The patient’s response to treatment should be evaluated by assessing their symptoms, vital signs, and laboratory results.
Nursing Considerations
The nurse plays a vital role in managing fluid and electrolyte imbalances. Nurses should assess the patient’s fluid balance and electrolyte levels, monitor the patient’s response to treatment, and provide patient education.
Top FAQs
What are the common causes of fluid and electrolyte imbalances?
Fluid and electrolyte imbalances can arise from various factors, including dehydration, excessive fluid intake, electrolyte loss through vomiting or diarrhea, kidney dysfunction, and hormonal imbalances.
How are fluid and electrolyte imbalances diagnosed?
Diagnosis involves a comprehensive assessment of the patient’s symptoms, medical history, physical examination, and laboratory tests. Blood and urine tests are essential for evaluating electrolyte levels and fluid status.
What are the principles of treatment for fluid and electrolyte imbalances?
Treatment aims to restore fluid and electrolyte balance by administering fluids, electrolytes, or a combination of both. The specific treatment plan depends on the underlying cause and the severity of the imbalance.